Investigative
Reporting
Award
“How Am I Going To Ask a Hospital for Help if the Abuse Happens in the Hospital?”: Sexual Violence in Hospitals and Doctor’s Offices
Find the original publication by Público here, find the original publication by Setenta e Quatro here.
Hospitals and doctors’ offices should be safe places, but they were not for the 47 women Setenta e Quatro spoke to. They were subjected to sexual abuse by doctors, nurses, and operational assistants and live with that trauma to this day. How has this happened over the past two decades? What are the failures of the system? Of the Justice? Of the Hospitals?
by Ana Patrícia Silva, Setenta e Quatro
She had been having unbearable menstrual pain for many months. The best solution was really to go to the doctor. She went to one appointment, then to a second. The doctor’s behavior did not arouse any suspicion in her; I would even say that the consultations were trivial. He prescribed medication and the pain stopped. But the success of the treatment required a third visit. Sandra booked it for 2023.
It was scheduled for 4 pm. It was the third time Sandra had been to that private practice in the Lisbon Metropolitan Area. She had started a treatment that was having positive results and for the first time the bleeding (and pain) had stopped. Sandra has endometriosis. It is a disease in which the endometrial tissue – the tissue that lines the uterus – grows outside the uterine cavity. It affects one in ten women of childbearing age and causes pain and possible bleeding. “Despite the pain, I was happy that something positive was happening,” she says.
She went into the office and the doctor told her to go to “the little room,” a specific room for exams. He wasn’t supposed to do tests: The appointment was for a discussion about the success of the medication. In that room, the doctor asked Sandra to take off her blouse. She was not wearing a bra.
She lay down on the couch and the doctor approached. “He brought his hands to my breasts and started groping them,” Sandra recounts. “He wasn’t supposed to examine my breasts, I hadn’t complained at any point.” For her, the type of touch was sexual, not clinical. “His gaze never crossed with mine, but I know and felt that something was going on and I wasn’t sure what it was about.” Sandra froze, or as mental health professionals say, froze. Not knowing where to look, she fixed her attention on the blue walls of the office and stayed that way, static, until the end of those two minutes that “seemed like hours” to her. It was the same blue that she used to draw pictures of doctors’ offices as a child; she liked to draw office rooms and doctors seeing patients. It’s a detail that she won’t forget now.
“Then he asked me if I had [pubic] hair on my vagina.” Sandra said no with her head. “He gestured with his hand for me to take off my panties — I had my pants undone — touching my crotch,” she explains, uncomfortable. Not knowing how to react, feeling repulsion, she turned to her left side, but the doctor, not realizing or ignoring this sign, continued. He insisted even more.
“He insisted that I take off my pants, because it was necessary to do a pelvic ultrasound on me with an endovaginal probe.” The decision to have this examination was made on the spot, Sandra says, since neither the ultrasound machine nor the necessary materials were previously prepared. But Sandra obeyed. She undressed and the next thing she knew the doctor had already inserted the probe, without even wearing gloves. “It was only yesterday that I realized that the machine wasn’t even on,” she says via video call three weeks ago.
The doctor never looked her in the eye. “He looked at the computer, changed the subject, and the appointment was over,” says the woman in her late 30s. What remained from this appointment was a prescription that itemized three packets of the medication she would have to continue taking. She never had access to the report of the supposed examination, nor did it ever appear in her medical file. It is as if it never happened.
Sandra’s case was not a “serious breach” of conduct, but, she says, sexual abuse. Generally, a gynecological ultrasound is not a test that is done routinely. “But there are many gynecologists who in private [offices] do the exam in the context of consultation, almost as an objective examination,” explains a gynecologist-obstetrician who prefers not to be identified for fear of reprisals.
Sandra has suffered a “hideous malaise” since the day she suffered the abuse. “With each passing day, the disgust I felt for myself was indescribable.” It took her a few days before she told her husband what happened: “I was abused.” Only after two months of therapy was she able to acknowledge it out loud.
Consecutive baths followed. “I felt so dirty,” she admits. Her husband couldn’t understand why she was constantly washing herself.
The act allegedly committed by the doctor falls under the crime of sexual coercion, as defined in Article 163 of the Penal Code. Sandra can still file a complaint. She has two months to do so until she reaches the maximum limit allowed by law: six months. She has been advised to do so by her psychologist and her husband, but the fear and shame she feels take up a place that still remains unattainable.
What is hidden when the door closes
Sexual violence in hospital settings and doctors’ offices exists. Although there is little consistent public data on sexual abuse committed by doctors, nurses, and operational assistants, Setenta e Quatro heard the story of Sandra and 46 other women survivors of sexual abuse (coercion or rape) in hospitals, public and private, and doctor’s offices.
All of these women state that there was never consent. Of the 47 women we heard, who were sexually abused between 2000 and 2023, only 14 gave us permission to use their testimonies in this research, which we will recount in the coming weeks. The remaining 33 stayed with exploratory interviews: the fear and emotional vulnerability they were subjected to in remembering the trauma was enormous. They didn’t want to go through it. They did not want to expose themselves, much less denounce their attackers for fear of being discredited. It is also for this reason that the names of the women subjected to these abuses are fictitious, to which we add reasons of privacy and legal protection. The crimes of coercion and rape are semi-public, that is, a complaint by the victim is required, but the authorities and public officials are obliged to report them to the competent authorities.
Over the last 12 months, we’ve spoken to specialists and legal representatives, doctors, nurses, operational assistants, mental health professionals specializing in Sexual Violence and Post-traumatic Stress, NGOs, researchers, professional associations, unions and leaders of associations to understand how all these women survivors, victims and patients remain unprotected in health services in Portugal. But, above all, how can these abuses to women’s sexual freedom and self-determination be fought and prevented?

Author: Rafael-Medeiros
We analyzed case by case, spoke with people close to the survivors, consulted court cases, read national and international reports, and looked at the few numbers of complaints and claims that exist about this context that has had a significant increase since 2015.
Of the 14 accounts we heard and were allowed to tell, three women filed complaints, but only two went to court, resulting in the conviction with a suspended sentence of a nurse. This was not the only court case to which Setenta e Quatro had access, but it was the only one in which we were able to speak with all the survivors involved.
The inexistence of protocols for action or prevention of situations of sexual violence between health professionals and patients reveals a “serious negligence” with which the subject is treated by Portuguese health institutions, say various specialists. Complaints do not always reach the competent entities and internal inquiries are not always made.
Besides this, there is no national protocol for prevention and procedures in cases of sexual violence between users and health professionals. The same does not happen with moral and sexual harassment among health professionals: Each Health institution decides internally how to proceed when a health professional sexually violates a user, but by law it must open an internal investigation and report the complaint to the judicial authorities.
The same happens in Justice: from complaint to conviction, the process is very long. And because of this, many victims end up giving up or not coming forward at all — often the lack of material evidence leaves them in judicial limbo. There are no surveillance cameras inside health institutions (they are not allowed by the privacy law), material evidence is often not collected within the legal 72 hours, this is when there are material traces and in case they return to the place where they often suffered the abuse. Not all hospitals have rape kits prepared to collect evidence and this can result in women sometimes having to travel hundreds of miles to other health facilities.
In the case of the archipelagos of Madeira and the Azores, “the reality is much more difficult.”
Even so, Teresa Maria Magalhães argues that it all depends much more on the “victim than on Forensic Medicine”. “The victim doesn’t even need to file a complaint; if she wants to, she goes directly to the hospital’s emergency department, and the hospital should call the medico-legal expert. But if there are delays, it’s because most of them don’t arrive within the window of opportunity that we consider to be the adequate time to safely collect the evidence”, reiterates the professor of the Department of Public Health, Forensic and Medical Education at the Faculty of Medicine of the University of Porto. But these traces do not always exist. And these women survivors don’t always manage to get there.
Another possibility is to go to a Crisis Care Center, such as the EIR – Emancipation, Equality and Recovery Care Center, coordinated by UMAR, but there are only two in Portugal: in Porto and Lisbon.
Besides all these obstacles, the recognition of the abuse by the victims is a painful process. It involves phenomena of guilt, social stigmatization and even shame. The questions they ask themselves are constant: why they didn’t prevent or do something to prevent the abuse becomes a dead end.
“An issue that is given little relevance and that is more or less proven both in other European countries and in Portugal, and this is a similar physical phenomenon: many times the women do not present traces, because they enter in that frozen state, I will use the English expression: the freeze,” explained Helena Leitão, Prosecutor of the Republic who finished at the end of May her second term as a member of the Group of Experts on Combating Violence against Women and Domestic Violence (GRÉVIO) of the Council of Europe. “They authentically freeze, and that was often used by the opposition, because if there is no trace, it means there is no counter, almost as if it is ‘the woman’s fault’.”
Violence against women is widespread throughout the European Union: “one in three women suffers from sexual violence,” reads the directive proposed to the European Commission in March 2022 on combating violence against women and domestic violence.
A study done by the Emancipation, Equality and Recovery Care Center (EIR), coordinated by UMAR and to which Setenta e Quatro had first-hand access, goes even further: if health professionals, due to their proximity to patients, are in a strategic position to detect risks and identify possible victims of violence, 73.2% of the 325 respondents said they did not feel safe to respond to a request for help from a victim of sexual violence.
Asked whether they had specific training in sexual violence to intervene in such situations, 93.8% of the respondents answered they did not. In addition, 73.2% responded that they did not know about specialized support services for victims of sexual violence, says the study The Challenges in Intervening with Victims of Sexual Violence: A survey of professionals, which will be made public in the coming weeks.
Prescribing a stigma that makes sexual violence invisible
“Who would believe me?” is a question that soon comes up in the cases we heard: all the victims and women survivors we spoke to who did not press charges, citing the status that abusers have and the profession they work in (doctors, nurses, but also operational assistants) as the main reason for giving up. And the few women who did press charges felt at some point in the process that their word would be challenged, because it would always be the word of “a woman against that of a doctor or nurse,” or because they considered “something like this unlikely to happen inside a health care institution.”
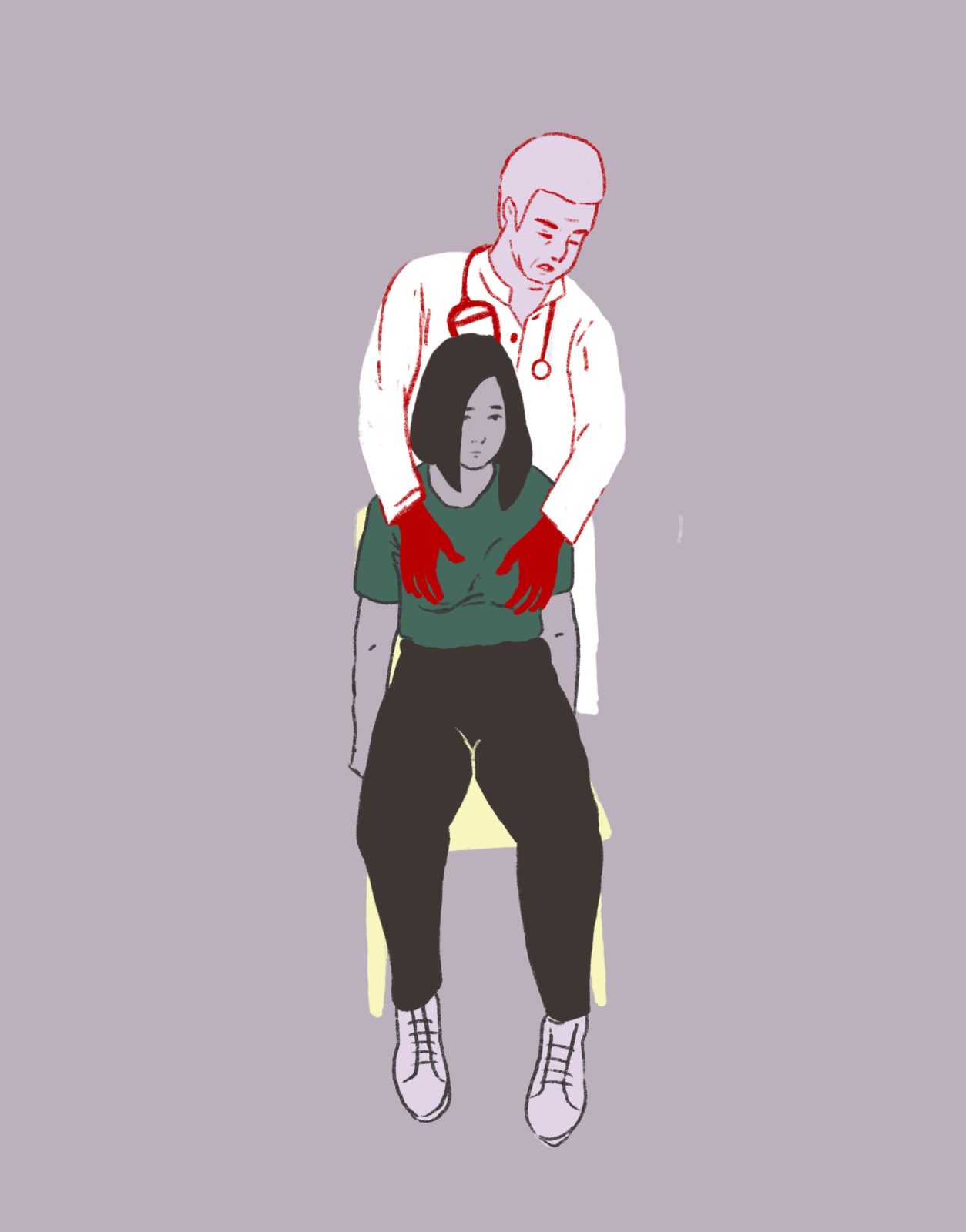
“There are no professions or social statuses immune to sex offenders,” reiterates Catarina Barba, a specialist in Sexual Violence and Post-Traumatic Stress to Setenta e Quatro. There is an urgent need for social and cultural deconstruction: “it’s not because a doctor who supposedly ‘protects’ us, who ‘takes care of us’, who ‘studies hard’, stops being a potential sexual aggressor – or any other health professional”, she says.
The number of complaints from users reaching the Health Regulatory Authority (ERS) warns of this: complaints about violence, aggression and/or harassment have increased dramatically since 2015. In 2022, the total number of complaints was 149: 28 cases in private hospitals with hospitalization, 15 in private hospitals without hospitalization, 79 in public hospitals with hospitalization, 19 in public hospitals without hospitalization, seven in “social” (nursing homes or long-term/palliative care) and one in “social” without hospitalization.

Author: Rafael-Medeiros
Less than six months have passed since the year 2023 began and 58 complaints have already been filed, which is 69% of those of the previous year.
This reality was even more nebulous until 2014, when ERS started receiving complaints and claims from users against health professionals. However, the health regulator does not discriminate, because of the privacy law, in its statistics the situations of sexual violence, grouping them under the same heading: “violence, aggression or/and harassment”.
In statements to Setenta e Quatro about what procedure is carried out after receiving a complaint, it replied that, “when it detects evidence of non-compliance and fundamental requirements or procedures for patient safety, it proceeds to a more in-depth evaluation of the situation, through specific diligences with the providers and/or proceeds to the opening of a new process of inquiry, evaluation or even administrative offense.
As far as public hospitals are concerned, the investigation process is the responsibility of the Inspectorate General of Health Activities (IGAS). Setenta e Quatro insisted for several months with IGAS to be able to understand how many of the complaints resulted in the opening of an investigation and, of these, how many in court cases, but we did not get a response until the publication of this investigation.
Over the last month, Setenta e Quatro tried to find out from the Ministry of Health if it was aware of the complaints, what type of procedures are opened in hospitals, and what measures or regulations existed, but it did not get a response until the publication of this investigation.
If in the last decade the numbers have been growing with the ERS, the same is true both in number of cases and in number of criminal complaints. Let’s look at the Annual Homeland Security Report (RASI) of 2022. When it comes to serious violent crime and sexual crime, the report only highlights child sexual abuse (including child pornography) and the crime of rape.
Published in late April, the report indicates that there were 519 recorded cases of rape in 2022 alone. That’s a 30.7% increase compared to 2021, when there were 397 cases, a 72% rise since 2015 – there was also a peak in 2019 with 431 cases.
If the cases seem rare at first glance, the director alerts to a reality that is worrying: the survivors, victims of sexual violence, who contact the service center have a very different number compared to those of domestic violence. The center received 153 complaints of sexual violence in 2022, and was only aware of one case in a hospital setting.
“What we have noticed is that because sexual violence is still a very invisibilized violence, women do not seek help from the center. There is a lot of stigma,” adds Marisa Fernandes, a psychologist at UMAR’s service center and one of the authors of the report on the challenges of intervening with victims of sexual violence. The number of requests for help has indeed increased, but this increase has not been observed in the opening of legal proceedings or even in effective monitoring of survivors, say Marisa Fernandes and Ilda Afonso.
Although 154 countries have passed laws on sexual violence, they do not always apply the internationally implemented standards and recommendations. Portugal is one such case. “The Council of Europe since 2008 has recommended the existence of at least one Crisis Center for every 200,000 women and currently there are two specialized centers for women victims of sexual violence, one in Porto and another in Lisbon,” says Marisa Fernandes, with Ilda Afonso corroborating it.
“It is notorious that both in the process of denunciation and in the support to victims there are failures and difficulties in providing answers, especially by the professionals who intervene directly with the victims. It is necessary to review intervention practices, increase the number of specialized care and follow-up responses and train professionals who intervene in the field of sexual violence,” warns Ilda Afonso.
If sexual violence in hospital settings is seen as “isolated acts” because of the scant numbers that are publicly revealed, it becomes even more difficult to prove how in these cases a person’s trauma can “link the victim to the aggressor.” “There may even be ‘just’ something in the treatment that makes us feel uncomfortable, but we were. Why? Because we need the doctor, we need that consultation, we need that treatment that only ‘that’ person can define”, stresses psychologist Catarina Barba, a specialist in Post Traumatic Stress.
Rui Ferreira Nunes, a psychologist who has worked extensively with people who have suffered sexual abuse, stresses that in clinical terms we know that there is a compulsion to repeat. “A person who has been abused may be abused again in a context that somehow replicates the experience of the first abuse. In a situation where there is a power differential, the person is somewhat at the mercy of the other, since they are usually in a position of vulnerability.”
The psychologist’s consideration is not at all distant from what Catarina Barba tells us about such acts happening in hospital settings. All these circumstances “discredit a woman: the one who was touched and the one who was raped. And it discredits her, “especially in a hospital setting where other people circulate, where there is the awareness and the feeling that one is not alone and at any moment someone might see or hear,” Barba concludes.
A patient’s word against a doctor’s
In her home in the central region of the country, Paula tells how being a mother is a challenging process. Ten years later she realized what had happened to her: “I was sexually abused by a doctor who was 20 years older than me.”
“Therapy helped,” she begins by saying by video call.
One summer, when she was 20, she decided to take her mother’s suggestion and went to her gynecologist and had two appointments. Even then she suspected she might have endometriosis, but she had to wait months for an appointment at the public hospital in her area of residence. Worried, she wanted to be examined as soon as possible, because the menstrual pains were very strong.
The medical office was divided into two parts: the place by the window where the doctor sat with his back to his desk with his computer and some important tools. On the opposite side was a small place reserved by a curtain, around a couch, which clustered on the left side a small island of medical instruments and the ultrasound scanner.
Paula entered, took about five minutes to explain to the doctor what was going on, and he asked her to lie down on the bed to examine her. “I was being watched by him, on the stretcher, and I asked him if it was normal to have pain during [sexual] penetration,” Paula says. What followed left Paula not knowing what to do and how to react: “He started penetrating me with his fingers and kept, over and over, trying to give me an orgasm.” She didn’t have one.
He kept going and she couldn’t react, the “shock was so great” that Paula remained inert, completely blocked, without moving. “I just wanted it to be over so I could get up and leave,” she admits, anguished. After that, she can’t remember if she said anything else to him. But she does remember one detail that haunts her to this day: he wasn’t wearing gloves. “I panicked,” she says.
This case touches on several issues raised in this investigation. Let’s start with gloves. The standard issued in January 2012 by the Directorate-General of Health (DGS) — a joint proposal between the Department of Quality in Health, the Program for Prevention and Control of Infection and Antimicrobial Resistance, and the Medical Association — leaves no room for doubt. “Gloves must be worn when contamination with blood or other organic fluids is anticipated,” reads the document. In other words, gloves must be worn when touching mucous substances, because they secrete fluids. Anything of this nature cannot be touched without some kind of protection.
In 2009, the World Health Organization (WHO) also recommended it in the Glove Use Information Leaflet. The document reads: “the use of medical gloves is recommended to reduce the risk of health professionals’ hands becoming contaminated with blood and other body fluids.”
But these are far from being unique cases of doctors not wearing gloves when examining patients. All the reports from women we heard about the specialty in Gynecology reported not having been examined with gloves. And this data is relevant because it shows the predominance of a “sexualization of an act that is clearly premeditated,” says Catarina Barba, the psychologist in Sexual Violence and Post Traumatic Stress.

Author: Rafael-Medeiros
Paula’s discomfort grew greater and greater as the doctor approached. She has become so immobilized that her legs are no longer strong. Her voice trembles as she struggles to remember what it took her a year to try to forget. She swallows hard. She knows that after this conversation she will spend a week anxious about having relived everything, but most of all about having verbalized it.
After what happened, Paula began to feel guilt. “Guilt for asking something that somehow could have induced some act.” The way she dealt for a decade with this memory — even if repressed in some details — was that “the doctor was showing me something that I was supposed to know and that was not sexual abuse, because the way they represented these moments in the movies was something violent, with a stranger, where a person does not give consent,” she adds.
For Marisa Fernandes, this is a “belief” that needs to be deconstructed. The number of rape crimes committed by strangers is lower, as we verified in the RASI, 36.3% of cases in 2022. “Rape and abuse cases are perpetrated less and less by strangers, we need to demystify this belief that the culprit is a man standing there on a corner, ready to attack the victim. When, in fact, the aggressors walk among us. They are people who transmit this confidence and in whom we trust to a certain extent,” explains the psychologist.
Unlike Sandra, Paula was not alone. Her mother had accompanied her and was waiting for her in the waiting room. She was also the one who encouraged Paula to talk to Setenta e Quatro about what had happened to her. “I feel safe doing this for me and for her,” Paula says, as she joins her hands with her mother’s and adjusts a bracelet.
“As soon as I saw her [leaving the office room], I knew something bad had happened,” shares her mother. Her eyes filled with tears as she recalled one of the most traumatic episodes in her daughter’s life. “I ran to get her, she was very disoriented. She was limping, she almost fell. When we got in the car, she started rocking back and forth, crying hysterically,” she continues in anguish. The mother didn’t know what to do. Paula just asked them to leave. She couldn’t be there.
Since then she has never been back to a male gynecologist, has never been seen by male doctors, not even in other specialties, and is extremely anxious every time she thinks about going to a hospital, to a doctor’s office, or even about having tests done. Paula had her daughter with much fear and caution. The doctor who accompanied her during pregnancy was a long-time friend and all the obstetric exams were done with professionals she knew. Otherwise “I would not have returned to a hospital or a doctor’s office.”
Taking a denunciation forward is a process that carries several complex stages and, for this reason, many victims end up giving up or not going forward at all. “These are extraordinarily fragile and painful crimes for the victims and for all the actors who have to come into contact with them,” explains Helena Leitão, a prosecutor who is finishing her second term as a member of the Council of Europe’s Group of Experts on Combating Violence against Women and Domestic Violence (Grévio).
Sandra’s and Paula’s stories are two of the 47 collected by Setenta e Quatro against doctors, nurses and operational assistants from hospitals (public and private) and private practices. The vast majority of health professionals (doctors and nurses) have not been removed from their positions, even when there are lawsuits in court.
Paula’s mother encouraged her to go ahead with the complaint, but the feelings of guilt and shame weighed heavily again: they gave up because they realized it was a “one-way street.” “When I tried to figure out what to do, a lawyer friend said she wouldn’t stand a chance.” It was the word of Paula, then 20 years old, against that of the doctor, a socially respected professional.
Author: Rafael-Medeiros
The unthinkable for any victim of sexual violence happens, and not infrequently in Portugal: being abused in the place where you should feel safest – in a hospital or doctor’s office. The testimonies, the numbers, the legal implications and the stigmas associated with a problem that has been in the news in recent weeks.
by Cláudia Marques Santos, Público
Manuela left the emergency room in a hurry, but in an effort, with small steps. They even made her sign a waiver and she walked out the door. She couldn’t stay there for another second. Two months ago, Manuela was lying on a stretcher in the emergency room of a public hospital in Portugal’s Centro region because of hypothermia – Manuela is immunosuppressed – when she recognised the voice of the nurse who raped her, she was 16 years old. “I was in the emergency room for seven hours. At shift change, I recognised the voice,” says Manuela, now 34. She had never been back to that emergency room again. But this time she hoped that her rapist was retired. She pretended to sleep, pulled up the blankets, and covered her face with one arm. The nurses stopped in front of the bed where she was. “If he had any doubts about who I was, he didn’t anymore. When I was sure he was far away, I called the doctor and said I wanted to leave,” Manuela explains, noting that the doctor advised her against it because they needed to do more tests. “While they went to get the consent form, he passed my stretcher seven or eight times, teasing me.” Manuela is sure he recognised her. She hid the catheter for fear that he would take it out. She got up slowly because if she fainted, she would stay in hospital. She started walking as best she could and got out of there. She removed the catheter herself, at home. “I thought I’d got over it and it turned out that everything was still inside.”
Publico (c) Joana F. Bastos
“He” is the nurse who raped her 22 years ago. It wasn’t the first time that Manuela had tried to kill herself by taking an excessive dose of pills. Autistic, Manuela was very thin and was constantly bullied by her classmates at school. Her relationship with her mother didn’t help either. At the hospital, her stomach was pumped, and she was put in a ward to recover. A man in scrubs approached her, he had a name written on his lapel, which she still remembers today, as well as his face, voice, and smell. “I was in a room with more beds and this man took care to look around before entering,” says Manuela. “It was the kind of conversation he approached me with… to see how I would react if I would shout, push him. He was trying to understand who he was dealing with. And he realised that there was someone there who was extremely vulnerable. ‘You deserve to live’ and he petted my hair.” He sedated her. She woke up the next day with blood and pain in her vagina.
Numbers on the rise
The act perpetrated by this nurse may constitute several crimes: rape (foreseen and punishable by article 164 of the Penal Code [CP]), in which there was vaginal copulation or the introduction of objects into the vagina; sexual abuse of a person incapable of resistance (article 165 of the CP); sexual abuse of a person in hospital (article 166 of the CP); and, as Manuela was 16 years old at the time of the events, sexual abuse of minors – between 14 and 18 years old – who are dependent or in a particularly vulnerable situation (Article 172 of the Criminal Code) can also be considered to have taken place.
Manuela still tried to file a complaint, but gave up when her mother wasn’t allowed into the Public Prosecutor’s office, where the abuser and his lawyer would also be.
There have been several news reports about recent cases of rape and sexual coercion. This Wednesday, for example, there were many reports about a radiologist with a private practice in Bragança who was brought before an investigating judge accused of two counts of rape. In 2022, the Health Regulatory Authority (ERS) received 149 complaints of “violence/aggression/harassment”, without distinction: 28 cases occurred in private hospitals with inpatient care; 15 in private hospitals without inpatient care; 79 in public hospitals with inpatient care; 19 in public hospitals without inpatient care; 7 in “social” care (nursing homes or long-term/palliative care); and 1 in “social” care without inpatient care.
In the last decade, the number of rapes has been growing, both in terms of cases and complaints. The recently published Annual Internal Security Report (RASI) for 2022 indicates that in 2015 there were 375 cases of rape and in 2019, 431 cases. In 2022, there were 519 cases, which means an increase of 30.7% compared to the previous year (397).
As for complaints from victims of aggressors who are health professionals – and according to ERS data – while 58 complaints were filed in 2015, this number has already been equaled in 2023 and up to May. “It should be noted that (…) the ERS is carrying out a more in-depth assessment of the situation, through specific steps with service providers and/or the opening of a new investigation process,” the ERS replied in writing, along with the latest figures. PÚBLICO insisted on finding out from the General Inspectorate for Health Activities, which is responsible for taking steps when complaints are lodged with public hospitals, how many of these complaints resulted in an investigation being opened and, of these, how many went on to trial. There was no reply.
For this work, we contacted 47 victims of sexual abuse – coercion or rape – in a hospital setting, both public and private, or in a doctor’s surgery. Of these 47, only 14 agreed to share their experience. The remaining victims stuck to exploratory conversations and gave up talking to us: all of them out of fear – of exposure, of possible reprisals – and many out of an emotional inability to live through what happened again.
Of these 14 victims, three filed complaints, two of which were charged and tried in court and resulted in the perpetrators being sentenced to suspended prison sentences. All the victims we spoke to who didn’t press charges mentioned the “social status” of the abusers – doctors and nurses – as the main reason. Their word would “always be worth more” in court than theirs. But there are other causes: the coldness of the rooms in hospitals and police stations to deal with them, the lack of training for professionals to deal specifically with their situation, and also the legal time to file a complaint, which is very short. Victims only have six months to do so. “How am I going to ask a hospital for help if the abuse happens in the hospital?” asks psychologist Catarina Barba. “And sexual violence always has these characteristics: it’s someone in a relationship of power – be it a parent, a teacher, a neighbour, the babysitter, the doctor.” This psychologist specialising in sexual violence and post traumatic stress makes a point of stressing that there are no professions or social statuses immune to the profile of a sexual aggressor. “But we have these prejudices: a doctor is ‘someone who looks after us’, who ‘protects us’. Someone who has ‘studied a lot’ and therefore ‘has a different way of being’,” she adds. “This skews our ability to understand that this doesn’t mean that a doctor can’t be a sexual aggressor.”
The victim, from trauma to awareness
The first thing her mother told her about the psychiatrist she had just been referred to was that he was known for being a womaniser. Her father had committed suicide when Sara was 13, because her mother wanted to separate, and from the age of 15, Sara was regularly sexually abused by her stepfather. When she went to college, she met a boy and they started dating. Sara says she used this “ruse” to try to get rid of her stepfather. She remembers the terror she felt whenever she was left alone at home with her mother’s new partner. He wasn’t working at the time. All she could think was: “Let’s get this over with”, so that she could free herself from the feeling of terror for the rest of the day. “It was as if I knew I would just stand there, static and… just waiting for it to be over. There was no subtlety there.” She calls it the “terror without a name”.
When she was 19 or 20 – she can’t remember exactly – Sara and her boyfriend broke up. “I was devastated. I’d been going through that violence for years,” says Sara, now 48. We’re in the consulting room of her current psychologist, whom she made a point of accompanying for this interview. “For the first time, I really fell apart.” She went to the psychiatrist her mother suggested, “well known in the area”, with a private practice in the Lisbon Metropolitan Area. He’s no longer alive. She was given medication and Sara got better. “He was a very cultured person,” she describes, explaining her fascination with the man: “He spoke to me about things that were much more erudite than people my age.” Once, the psychiatrist took the book Moderato Cantabile by Marguerite Duras and started reading it to her during his consultation. “It’s a book about a married woman from the early 20th century who starts going to a tavern where she meets a man and drinks glasses of wine.” She remembers that, sometime later, she was walking down the street and trying to convince herself that it wasn’t the same as what had happened with her stepfather. “But what I felt was the same. So I didn’t feel well, I didn’t,” Sara admits. “Obviously because it wasn’t really a free choice on my part. I was manipulated and led to a certain place to make it happen.” It wasn’t until she was 30 that she realised it was abuse.
This abuse is defined as a crime in Article 165 of the Penal Code and concerns “anyone who engages in a sexual act with a person who is unconscious or otherwise incapable of resisting, taking advantage of their state or incapacity.” In court, judges even question why there are no physical marks of a struggle on the victim’s body. In a dangerous situation, present in any violent act, our brain reacts automatically to protect us, explains psychotherapist Rui Ferreira Nunes. “There are three possible responses on the part of the victim: the fight, which is a reaction of struggle towards the dangerous stimulus; the flight, almost like a reaction of flight in the face of danger; and the freeze, seen as a reaction of paralysis in the face of the dangerous situation, which is often questioned from a legal point of view,” says Ferreira Nunes. “These are behaviors that can be reproduced both during and after the abuse.” Juliana feels ashamed to have been a victim of sexual coercion in a private hospital in the central region of the country. “I feel ashamed that anyone knows I was in a situation like that. Shame is the dread behind exposure.”
Juliana is now 32 and was abused by a doctor when she was pregnant at the age of 29. She has never been to therapy, although she is aware that she should have. “I thought it would pass. But I’m not getting over anything. To get over something, I have to go to therapy, to talk.” Juliana told us that the fact that she shared her story with us relieved her, in a way.” Awareness is always a complex and very time consuming process, I would even say delayed, for various reasons. One of them is the shame inherent in the situation. The victim often feels guilty about what happened, thinking they could have done anything to prevent the abuse: run away, said no,” explains Rui Ferreira Nunes. “Shame becomes a very toxic feeling.”
Some people take years to deal with the trauma. That’s why, from legal experts to Non-Governmental Organizations (NGOs) linked to victim support, the argument is unanimous: the maximum time of six months after the abuse to file a complaint is too short and the crime should not be semi-public, but public. “It’s absurd,” agrees public prosecutor Helena Leitão. “If the crime is public, it’s not even necessary to discuss the deadline for filing a complaint. It means that, as long as the crime doesn’t lapse – and a crime of this nature can take up to 15 years to lapse – the investigation can go ahead regardless of the victim’s or family’s wishes,” explains Helena Leitão. “The truth is that the victim may not want to press charges for various reasons, ranging from wanting to forget what happened to her once and for all, to the shame and guilt she mistakenly feels, to pressure from her family who may say, ‘we’ll be marked’. And even on the part of boyfriends or husbands, there can be a lack of understanding.”
One day, a few weeks into her pregnancy, Juliana had a headache and went to the health center. There, she was told that she should have already had her prenatal tests. As there was no immediate vacancy at the public hospital, she decided to pay for the ultrasound out of her own pocket and went to a private hospital, also in the central region of the country. “The doctor gave me the touch test, the test where he puts his finger in my vagina, and I was surprised,” says Juliana. “I thought this test was only done when a pregnant woman was about to give birth. But as it was the doctor, I didn’t question it.” He didn’t wear gloves. The doctor then asked her to get on the scales to weigh herself. As she passed him, he brushed his hand across her bottom and let it rest there for a moment. Juliana was only wearing the gown she had been given by the hospital. Juliana ended up pushing his hand away. “You think you can have 1001 reactions, like ‘I’d hit him’, ‘I’d make a fuss’, but I was paralysed.” She remembers the doctor’s lecherous smile well. As soon as she could, she left the hospital. She didn’t even take the test. “If I was thinking of having a second child, I’m not anymore,” she confesses. “I can’t go back to that place, the place of being pregnant.”

Publico (c) Joana F. Bastos
Abuse situations are similar to panic situations, explains Rui Ferreira Nunes. “The person doesn’t know how to react. They’re taken by surprise and their brain stops thinking, stops using its cognitive functions in the direction of action, because emotionally it’s blocked.” Catarina Barba says that sexual violence is something that takes away all sense of control.
Little support for the victim, little training
Porto’s Service Center of the NGO UMAR – União de Mulheres Alternativa e Resposta (Union of Alternative and Responsive Women) only became aware of one case of sexual abuse in a hospital setting last year. UMAR’s president and psychologist, Ilda Afonso and Marisa Fernandes, warn of a worrying reality: the number of women who are victims of sexual violence who contact the service centre is very low compared to victims of domestic violence. Marisa Fernandes ventures an explanation: “What we’ve noticed is that, because sexual violence is still very invisible, women don’t seek help from the center. There’s a lot of stigma.” Marisa Fernandes is also one of the authors of the UMAR report entitled The Challenges of Intervening with Victims of Sexual Violence: A study with health and education professionals in the district of Porto. Dated March, this report – not yet available online – presents the results of a survey of health professionals in that district, in which 29.7% say they have major problems with the external articulation of the action protocol defined for situations of sexual aggression and 26.1% report difficulty in identifying the situations themselves. When asked if they had specific training to intervene in this type of situation, 93.8% said they had not. “It is notorious that, both in the process of reporting and in supporting victims, there are shortcomings and difficulties in providing a response, especially on the part of the professionals who intervene directly with the victims. There is a need to review intervention practices in the field of sexual violence, increase the number of specialised care and follow-up services and train professionals,” argues Ilda Afonso.
The European Council Convention on preventing and combating violence against women and domestic violence, signed in May 2011 in Istanbul (Istanbul Convention), is a binding international legal instrument that establishes a legal framework of measures to be implemented by participating states to protect women from violence. This convention was ratified in Portugal in February 2013 and entered into force in August 2014.
“Since 2008, the Council of Europe has recommended that there should be at least one crisis center for every 200,000 women. In Portugal, there are currently two specialised centres for women victims of sexual violence, one in Oporto and the other in Lisbon,” denounce Ilda Afonso and Marisa Fernandes.
Until the end of last month, public prosecutor Helena Leitão was one of the fifteen independent experts responsible for monitoring the application of the Istanbul Convention in the various member states, as part of the so-called GREVIO committee. “When I came back from the meetings in Strasbourg and started to see Lisbon from the plane, I admit that I was thinking almost unconsciously: ‘for a few weeks I’m going to be better with myself and with life’, because I’m aware that, unfortunately, the situation in the other countries of Europe is no better than in Portugal.”
The Shadow Report presented in 2022 to the GREVIO committee by the NGOs Associação de Mulheres Contra a Violência, Plataforma Portuguesa para os Direitos das Mulheres and European Women’s Lobby, considers that – and taking into account the committee’s General Recommendation no. 35 – neutrality in laws is no longer acceptable. In her book Medusa no Palácio da Justiça ou uma História da Violação Sexual (Medusa in the Palace of Justice or a History of Sexual Violation), sociologist Isabel Ventura corroborates the presence of patriarchal culture in the law itself. “The difficulty (or even inability) to think of women as authors, decision makers and holders of an active sexuality that is not dependent on (and at the service of) male actions is continually present in the speeches of Portuguese penalises, before and after the 2007 penal reform. This is what Figueiredo Dias says, when he assures that ‘rape always requires the intervention of the male sexual organ’, or that ‘copulation is thus only the penetration of the vagina by the penis’, and even that ‘the common meaning of coitus requires a conjunction of bodies with other organs or with any objects’.”
Furthermore, the precept is that the intensity of the crime is proportional to the victim’s reaction. “All this clearly indicates that the victim is still obliged to present antagonism. They are only exempted from this imposition if they are prevented from doing so, in other words, if they are unconscious or semi unconscious,” the book also states.
Lack of harassment kits in hospitals
“I only realised yesterday that the machine wasn’t even on,” Sandra said via video call three weeks ago. In April last year, she went to a gynaecologist with a private practice in the Lisbon Metropolitan Area for the third time because of endometriosis problems. Endometriosis is a disease in which endometrial tissue, the tissue that lines the uterus, grows outside the uterine cavity and can spread to other organs. Sandra entered the office and the doctor asked her to go to the examination room. He told her to take off her upper garment and lie down on the couch. The World Health Organization recommends that two health professionals be present for gynaecological examinations, which was not the case. “He took his hands to my breasts and started to feel them,” says Sandra, 32. “I felt something was happening and I wasn’t sure what it was.” Sandra froze.
Publico (c) Joana F. Bastos
“Then he asked me if I had hair on my vagina.” Sandra nodded no. “He gestured with his hand for me to take off my underwear, touching me on the groin,” she explains uncomfortably. Sandra even turned to her left as a sign of refusal. “He insisted that I take off my underwear because I needed a pelvic ultrasound with an endovaginal probe,” a decision that, according to Sandra, was made on the spot, because nothing was prepared for that examination. She obeyed, took off her underwear and the next thing she knew, the doctor was inserting the probe without even wearing gloves.
Washing themselves because they feel dirty is a common reaction among victims of sexual abuse. This means that the presence of the abuser’s fluids in the victim’s body is drastically reduced. This examination is carried out by a forensic doctor, who is called to the hospital, and it is recommended that the victim comes forward within a maximum of 72 hours.
“Most of the victims don’t arrive within that window of opportunity that we consider to be the right amount of time to collect traces safely,” explains Teresa Maria Magalhães, coordinator of the Forensic Medicine and Forensic Sciences unit of the Department of Public Health Sciences, Forensics and Medical Education at the Faculty of Medicine of the University of Porto. “They often wonder if they’re going, if they’re not, and they come back three, four, five days later, sometimes much longer. And they come after they’ve urinated, after they’ve eaten, after they’ve washed themselves, washed their clothes, thrown their clothes away. After a series of things that have resulted in nothing less than the destruction of traces.” For adult victims, the law on medico-legal examinations stipulates that the doctor in the emergency room can receive the person and take the samples, explains this forensic medicine specialist. “And the person is seen at the Institute of Legal Medicine and Forensic Sciences the next working day. The material collected goes to the genetics laboratory.” But these cases carry a risk. “When forensic medicine specialists don’t take the samples according to the rules, they may not be done as well and sometimes a poorly taken sample, a poorly preserved sample or a poorly sent sample can be worthless in terms of evidence.”
From conviction to suspended sentence
She has passed her attacker several times in the street. Today, Carlota no longer looks away when she passes the nurse who abused her in the emergency room of the public hospital in a small town in the Alentejo region 14 years ago. Carlota filed a complaint, which went to court and resulted in a conviction. She believes that she only won the case because her abuser was the target of another lawsuit brought by Ana and Joana for the same reasons.
In a small town, Ana and, above all, Carlota were victims of threats and bullying. They were booed, called liars on the way in and out of court. They would pass Carlota’s house and shout abuse at her. His family also threatened her. They sometimes told her if she wasn’t ashamed that she was “ruining life” for the boy. The courtroom was always full. Seven years passed between the filing of the complaint and the judgment of the Court of Appeal – he appealed against the conviction at first instance.
One day, she began to lose strength in her legs. She went to the emergency room, taken by her sister. “You go to the hospital, and you feel safe. You’re sick and you go there to get well,” says Carlota. She begins: “The nurse came in and closed the curtain. I didn’t suspect.”
The nurse took blood from Carlota and then told her he was going to give her pain medication. In court, it was proven that she had been drugged. “We’ve lost our sight and hearing and all physical strength. We were blocked,” explains Carlota. “He warned me, saying: ‘Don’t worry, you’ll start to feel light and everything is fine. Just relax’. He left and then came back.” The nurse used Carlota’s hands to masturbate while repeating phrases like: “Do you like anal sex?”; “Do you like blow jobs?” in her ear. “I have the idea that I only had my eyes open, as if I was shouting, but I couldn’t do it. I’m sure that if he didn’t drug people, he wouldn’t touch anyone, least of all me,” she says assertively. “When he started touching my body, I thought: ‘I want to die right now’. And I felt a force in me that made me black out.”
Carlota was outraged as soon as she remembered what had happened to her in the emergency room, and was already in her sister’s car returning home. They immediately went back to the hospital to file a complaint. “I got there and told a nurse that I wanted to complain. She arrogantly told me to start talking while she tore up some paper to write it down,” says Carlota. “If I was already completely lost in my life, having that insensitivity killed me.” She filed a complaint and returned home. Her mother got the whole family together and all her uncles came home. “This was a huge wave of love for me. But at the same time, a huge shame.” Carlota took a shower, she felt dirty. The family decided that Carlota would go to the police. It was late at night when she entered a PSP police station. The officer, says Carlota, was in shock and felt her pain. He became her witness in court.
Later that night, he took her to hospital for a blood test. “They wouldn’t let my family in. So he stayed by my side the whole time, he never left me alone,” Carlota says emotionally. “When we got there, he said: ‘The victim made a complaint that she was sexually abused in this hospital in the afternoon and we wanted to do a blood test to see what kind of drug it is, because this counts in court’.” The doctor she told claimed that Carlota could have arrived at the hospital on drugs. “The policeman freaked out. He said it was shameless. They did urine and blood tests. “I went into the bathroom alone and this officer was always at the door. I felt safe.” Carlota spent three years in court. “They were the worst years of my life,” she says. She never walked alone and was always looking everywhere. “It was a mixture of shame, humiliation, revolt and injustice. All at the same time. Not least because he filed a libel suit against me.”
The Victim’s Statute, approved in September 2015 and in parallel with the Code of Criminal Procedure (CPP), establishes that the questioning of victims must be carried out by a person of the same sex, unless it is carried out by a public prosecutor or a judge. Measures must also be taken to avoid eye contact between victims and defendants in the courtroom. A particularly vulnerable victim can even give their statement in advance, recorded and used for “future memory”. “Until recently, judges understood that it was indispensable to the discovery of the truth for victims to repeat their testimony at trial. Fortunately, this practice is being reversed,” says public prosecutor Helena Leitão. “Things will tend to move in a positive direction. But these processes take time. Neither laws nor mentalities evolve quickly. There may also be a tendency for the legislator to seek to safeguard the stability of the certainty of the law, particularly criminal law and criminal procedure.”
Carlota felt a lot of shame in court. “I felt like I was being judged for being there. Everyone knew who I was, the exposure…”, she explains. Some people even spat at her as she left the hearing. “It was horrible in court. I could see the attacker from the front. I could see him laughing as I spoke. It was as if I was on a terrace.” Carlota’s case resulted in a conviction, a four-year suspended prison sentence and payment of compensation. The defendant appealed against the decision, but the Court of Appeal increased his suspended sentence to five years and the amount of compensation to be paid doubled.”It’s very rare for an aggressor’s first conviction in a criminal case to be a prison sentence,” says Helena Leitão. “Between a prison sentence or a sentence to be served in freedom, Article 70 of the Portuguese Penal Code is clear when it stipulates that preference should be given to the latter, whenever it ‘adequately and sufficiently fulfils the purposes of the punishment’. In other words, whenever a judge considers that it is sufficient for the defence of public order, as well as for the socialisation of the aggressor, to impose a sentence to be served in freedom,” explains the public prosecutor. “In systematic terms, the criminal law is structured like this: the perpetrator should be given a second chance whenever possible. But there are clearly cases and types of crime were giving a second chance is not justified. Above all, the victim has to feel that the legal and social system protects her.”
Carlota still suffers from vaginismus today. “There are causes of sexual problems in adult survivors that are related to the mind-body dissociation that occurred during sexual abuse, a defence that arises as a way of preventing pain during the sexual act, but which ends up also preventing pleasure,” explains psychotherapist Rui Ferreira Nunes. “Another mechanism is the loss of sensitivity in different parts of the body, as if they were anesthetised, particularly in sexual positions or practices associated with the abuse. They may even have vaginismus, pain on penetration, a psychological symptom, but which is felt as physical pain”, he says.
“I got vaginismus. It’s an emotional pain that’s stuck there, it’s not real,” says Carlota. “The body somatises. I’ve never been to the doctors to prove it, but I feel my body myself and I know my body before and after.”
* All the victims’ names are fictitious.
** The Ministry of Health and the Judiciary Police were contacted several times to answer questions from PÚBLICO and Setenta e Quatro, but we did not receive a reply by the time this text went to press.
Further Credits:
Rafael Medeiros, Joana F. Bastos, illustrations
Ricardo Cabral Fernandes, Sérgio B. Gomes, editor
Pulitzer Center







